Cervical Cancer Screening among Urban Women in Lagos, Nigeria: Focus on Barriers and Motivators for Screening
DOI:
https://doi.org/10.60787/njgp.v18i1.36Keywords:
urban Lagos, Nigeria, motivators, cervical cancer screening, BarriersAbstract
Background: Cervical cancer screening is known to be highly effective in reducing the incidence, morbidity, and mortality associated
with cervical cancer. However, the provision and availability of these screening services have not resulted into increased uptake of cervical cancer screening in many developing countries due to the interplay of several factors which influence women’s decision to undergo or not to undergo cervical cancer screening.
Objective: The objective was to assess the factors that serve as barriers and motivators for cervical cancer screening among urban women in Lagos, Nigeria.
Methods: A descriptive cross‑sectional study conducted among women attending an urban General Hospital in Lagos, Nigeria, using a structured questionnaire to assess their barriers and motivators for cervical cancer screening.
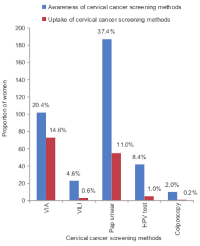
Results: Awareness and uptake of cervical cancer screening were low among women, accounting for 41.4% and 18.4%, respectively. The major factors motivating women to undergo cervical cancer screening were recommendation by doctor/nurse (53.3%), advice from friends/relatives (21.7%), and enlightenment by the media (20.7%). The major barriers to the uptake of cervical cancer screening were lack of awareness of screening methods (64.2%), lack of adequate information on screening methods (43.4%), and non-recommendation by doctors (41.4%).
Conclusion: The uptake of cervical cancer screening is low among urban women in Lagos, Nigeria. The lack of awareness and adequate information on cervical cancer and its screening methods were the major barriers to the uptake of cervical cancer screening, while recommendation by doctors/nurses and advice from friends and relatives were the major motivators for cervical cancer screening.
Downloads
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and
mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394‑424.
The Global Cancer Observatory: GLOBOCAN 2018 Nigeria Population and Cancer Fact Sheets; 2018. p. 1‑2.
Koliopoulos G, Nyaga VN, Santesso N, Bryant A, Martin‑Hirsch PP, Mustafa RA, et al. Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database Syst Rev 2017;8:CD008587.
Adegboyega A, Aleshire M, Linares AM. Examining cervical cancer screening utilization among African immigrant women: A literature
review. Int J Womens Health Wellness 2017;3:46. Committee on Health Care for Underserved Women. Committee opinion no 624: Cervical cancer screening in low‑resource settings. Obstet Gynecol 2015;125:526‑8.
World Health Organization. WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization; 2013: 1‑40
Catarino R, Petignat P, Dongui G, Vassilakos P. Cervical cancer screening in developing countries at a crossroad: Emerging technologies and policy choices. World J Clin Oncol 2015;6:281‑90.
Nygård M. Screening for cervical cancer: When theory meets reality. BMC Cancer 2011;11:240.
World Health Organization. Cervical Cancer Screening in Developing Countries: Report of a WHO Consultation. Geneva, WHO Press; 2002.
p. 1‑75.
Horan T. Women’s health. Screening in time saves lives. Nurs Community 2007;8:25‑6.
Guilbert E, Boroditsky R, Black A, Kives S, Leboeuf M, Mirosh M, et al. Canadian consensus guideline on continuous and extended
hormonal contraception, 2007. J Obstet Gynaecol Can 2007;29:S1‑32.
American Cancer Society. Global Cancer Facts & Figures 3rd ed. Atlanta: American Cancer Society; 2015. p. 1‑61.
Oluwole EO, Mohammed AS, Akinyinka MR, Salako O. Cervical cancer awareness and screening uptake among rural women in Lagos,
Nigeria. J Community Med Prim Health Care 2017;29:81‑8.
Onyenwenyi AO, Gugu GM. Strategies for the prevention and control of cervical cancer in rural communities: A Nigerian perspective.
J Community Med Prim Health Care 2016;28:77‑93.
Sowemimo OO, Ojo OO, Fasubaa OB. Cervical cancer screening and practice in low resource countries: Nigeria as a case study. Trop J Obstet Gynaecol 2017;34:170‑6.
Udigwe GO. Knowledge, attitude and practice of cervical cancer screening (pap smear) among female nurses in Nnewi, South Eastern
Nigeria. Niger J Clin Pract 2006;9:40‑3.
Onah HE, Ozugwu FO, Eze JM. Cervical cancer screening. A survey of current practice among Nigerian gynaecologist. Trop J Obstet Gynaecol 2001;18:78‑81.
McFarland DM, Gueldner SM, Mogobe KD. Integrated review of barriers to cervical cancer screening in Sub‑Saharan Africa. J Nurs
Scholarsh 2016;48:490‑8.
Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern
Ghana. Int J Womens Health 2015;7:31‑9.
Ndikom CM, Ofi BA. Awareness, perception and factors affecting utilization of cervical cancer screening services among women in
Ibadan, Nigeria: A qualitative study. Reprod Health 2012;9:11.
Lagos state Government. Abstract of Local Government Statistics 2016. Lagos Bureau of Statistics; 2016. p. 1‑94.
Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med 2013;35:121‑6.
Chinaka CC, Nwazue UC. Awareness of cervical cancer and its screening in Abakaliki, Nigeria. Afr J Cell Pathol 2013;1:47‑51.
Bakari M, Takai IU, Bukar M. Awareness and utilization of Papanicoloau smear among health care workers in Maiduguri, Nigeria. Niger J Basic Clin Sci 2015;12:34‑38.
Okunowo AA, Daramola ES, Soibi‑Harry AP, Ezenwankwo FC, Kuku JO, Okunade KS, et al. Women’s knowledge of cervical cancer and uptake of Pap smear testing and the factors influencing it in a Nigerian tertiary hospital. J Cancer Res Pract 2018;5:105‑11.
Bukar M, Takai IU, Audu BM. Determinants of utilization of Papanicolaou smear among outpatient clinic attendees in North‑Eastern
Nigeria. Afr J Med Med Sci 2012;41:183‑9.
Oche MO, Kaoje AU, Gana G, Ango JT. Cancer of the cervix and cervical screening: Current knowledge, attitude and practices of female
health workers in Sokoto, Nigeria. Int J Med Med Sci 2013;5:184‑90. 16
Awodele O, Adeyomoye AA, Awodele DF, Kwashi V, Awodele IO, Dolapo DC, et al. A study on cervical cancer screening amongst nurses
in Lagos University teaching hospital, Lagos, Nigeria. J Cancer Educ 2011;26:497‑504.
Idowu A, Olowookere SA, Fagbemi AT, Ogunlaja OA. Determinants of cervical cancer screening uptake among women in Ilorin, North
central Nigeria: A community‑based study. J Cancer Epidemiol 2016;2016:6469240.
Adanu RM, Seffah JD, Duda R, Darko R, Hill A, Anarfi J. Clinic visits and cervical cancer screening in Accra. Ghana Med J 2010;44:59‑63.
Al Sairafi M, Mohamed FA. Knowledge, attitudes, and practice rel ted to cervical cancer screening among Kuwaiti women. Med Princ Pract
;18:35‑42.
Mutyaba T, Mmiro FA, Weiderpass E. Knowledge, attitudes and practices on cervical cancer screening among the medical workers of
Mulago hospital, Uganda. BMC Med Educ 2006;6:13.
Wong LP, Wong YL, Low WY, Khoo EM, Shuib R. Knowledge and awareness of cervical cancer and screening among Malaysian women
who have never had a pap smear: A qualitative study. Singapore Med J 2009;50:49‑53.
Adamu AN, Abiola AO, Ibrahim M. The effect of health education on the knowledge, attitude, and uptake of free pap smear among female
teachers in Birnin‑Kebbi, North‑Western Nigeria. Niger J Clin Pract 2012;15:326‑32.
Rezaie‑Chamani S, Mohammad‑Alizadeh‑Charandabi S, Kamalifard M. Knowledge, attitudes and practice about pap smear among women
referring to a public hospital. J Family Reprod Health 2012;4:177‑82.
Francis SA, Leser KA, Esmont EE, Griffith FM. An analysis of key stakeholders’ attitudes and beliefs about barriers and facilitating factors
in the development of a cervical cancer prevention program in South Africa. Afr J Reprod Health 2013;17:158‑68.
Blake SC, Andes K, Hilb L, Gaska K, Chien L, Flowers L, et al. Facilitators and barriers to cervical cancer screening, diagnosis, and
enrollment in medicaid: Experiences of Georgia’s women’s health medicaid program enrollees. J Cancer Educ 2015;30:45‑52.
Isa Modibbo F, Dareng E, Bamisaye P, Jedy‑Agba E, Adewole A, Oyeneyin L, et al. Qualitative study of barriers to cervical cancer
screening among Nigerian women. BMJ Open 2016;6:e008533.
Ndejjo R, Mukama T, Kiguli J, Musoke D. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda:
A qualitative study. BMJ Open 2017;7:e016282.
Ebu NI. Facilitators and barriers to cervical cancer screening among HIV‑positive women in Ghana. Afr J Midwifery Womens Health
;12:93‑9.
Ndukwe EG, Williams KP, Sheppard V. Knowledge and perspectives of breast and cervical cancer screening among female African immigrants in the Washington D.C. Metropolitan area. J Cancer Educ 2013;28:748‑54.
Brown DR, Wilson RM, Boothe MA, Harris CE. Cervical cancer screening among ethnically diverse black women: Knowledge, attitudes,
beliefs, and practices. J Natl Med Assoc 2011;103:719‑28.
Garcés‑Palacio IC, Scarinci IC. Factors associated with perceived susceptibility to cervical cancer among Latina immigrants in Alabama.
Matern Child Health J 2012;16:242‑8.
Anaman‑Torgbor JA, King J, Correa‑Velez I. Barriers and facilitators of cervical cancer screening practices among African immigrant women living in Brisbane, Australia. Eur J Oncol Nurs 2017;31:22‑9.
Byrd TL, Chavez R, Wilson KM. Barriers and facilitators of cervical cancer screening among Hispanic women. Ethn Dis 2007;17:129‑34.
Published
Issue
Section
License
Copyright (c) 2024 Nigerian Journal of General Practice

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.