Vaccine Hesitancy in Nigeria: Contributing Factors – Way Forward
Main Article Content
Abstract
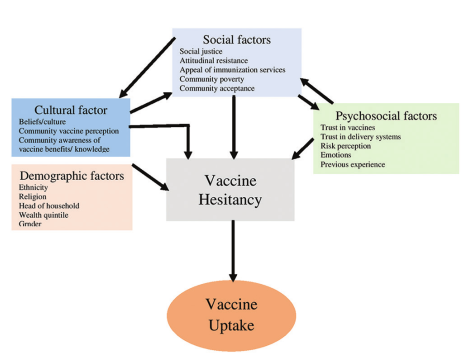
Vaccination coverage and program in Nigeria has continued to suffer setback in spite of various interventions. Vaccine hesitancy defined as a delay in the acceptance or refusal of vaccines despite the availability of vaccination services may be a cause of the poor trend in childhood immunization observed in Nigeria. The reasons why individuals hesitate or choose not to vaccinate vary across cultures and contexts. There is a need to develop context‑specific strategies generated from local research to reduce vaccine hesitancy and improve vaccination uptake in the country.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
References
Babalola S, Olabisi A. Community and Systematic Factors Affecting the Uptake of Immunization in Nigeria: A Quantitative Study in Five States. Nigeria; Abuja: Department of International Development; 2004.
National Demographic Health Survey. Key Findings. National Demographic Health Survey; 2008. Available from: https://dhsprogram.com›pubs›pdf. [Last accessed on 2019 Aug 26].
NDHS 2013 National Population Commission, Federal Republic of Nigeria. Final Report on Nigeria Demographic and Health Survey 2013.
Rockville, MD, USA: ICF International; 2013.
NPHCDA. Nigeria National Routine Immunization Strategic Plan (2013‑2015) Available from: http://www.nationalplanningcycles.org/sites/default/files/country_docs/Nigeria/ri_strategic_plan_combined_mahmud_draft_1.pdf. [Last accessed on 2019 Aug 26].
Wolfe RM, Sharp LK. Anti‑vaccinationists past and present. BMJ 2002;325:430‑2.
Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti‑vaccine movement: Influence, impact and implications.
Expert Rev Vaccines 2015;14:99‑117.
Ghinai I, Willott C, Dadari I, Larson HJ. Listening to the rumours: What the northern Nigeria polio vaccine boycott can tell us ten years on. Glob Public Health 2013;8:1138‑50.
SAGE Working Group on Vaccine Hesitancy Final Report. Available from: http://www.who.int/immunization/sage/meetings/2014/october/.
[Last accessed on 2019 Aug 26].
MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015;33:4161‑4.
Fine P, Eames K, Heymann DL. “Herd immunity”: A rough guide. Clin Infect Dis 2011;52:911‑6.
Betsch C, Bohm R, Chapman GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci
;2:61‑73.
Dubé È, MacDonald NE. Managing the risks of vaccine hesitancy and refusals. Lancet Infect Dis 2016;16:518‑9.
Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ; SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine
hesitancy – A systematic review. Vaccine 2015;33:4180‑90.
Dubé E, Gagnon D, MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015;33:4191‑203